
Helping doctors strike back against superbugs
Drug-resistant bacteria, originating from the overuse and misuse of antibiotics, kill millions of people each year – even more than HIV and AIDS, according to a 2022 Lancet study. Hundreds of thousands of these deaths are the result of commonly occurring infections that were previously treatable. This already worrying situation could become seriously bleak without more tools in our arsenal to fight this problem. Fortunately, scientists and engineers, such the University of St. Andrews’ Dr Robert Hammond, are on the case.
“I was the sort of child who would take objects apart. [Like taking] apart the microwave to get the magnetrons out, because you can build all sorts of things with those,” says Robert. Equally fascinated with biology and medicine, he ended up training as a microbiologist. He also spent time working for the Scottish National Blood Transfusion service and in hospitals. He marvelled at the centrifuges used to separate buffy coat (the mixture containing most of the white blood cells and platelets) from blood, but also observed workflows in hospitals that delayed patients receiving their results – lags, breaks, bottlenecks – many of which he believed were solvable problems.
One such workflow that Robert set out to address with his PhD research could have a huge impact in fighting antibiotics resistance. Antimicrobial susceptibility testing (AST) is used by doctors treating suspected bacterial infections to help them prescribe the right antibiotics. It involves exposing bacteria to different concentrations of a drug, or multiple drugs, to find the concentration at which the microbe stops growing – the minimum inhibitory concentration (MIC).
Machines used to analyse AST in the UK and around the world typically test samples of microbes against 12 broad-spectrum antibiotics, in a process that takes up to 48 hours. For the drugs tested, the doctor will be given a simple S (for susceptible) or R (for resistant) and will know which antibiotics will be effective, but won’t receive the exact MIC. If the microbe in question is resistant to all the drugs tested, the doctor will have to consider second- or third-line drugs to treat the patient.

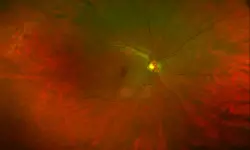
Drug susceptibility testing, used to detect drug-resistant infections of Mycobacterium tuberculosis © CDC, Unsplash
However, the problem with AST is that there can be a long delay before a result is obtained, meaning doctors must often prescribe an antibiotic before they are sure it’s the right one. Along with the several hours for the machines to perform their analysis, patient samples also must be cultured overnight in the lab first to grow a large enough (and pure enough) sample of bacteria to be analysed . In some cases, such as in a spinal fluid or blood infection, this total time of two or three days is too slow and, “these people are remarkably unwell, if not actually no longer with us at that point,” says Robert. “So that’s a big medical problem that could have a relatively straightforward engineering solution. That was something I wanted to look at, and what I ended up doing was creating this machine – a very, very rapid AST device.”
A death star targeting bacteria
Very early on in his PhD, Robert built the device, called a scattered light integrating collector (SLIC). When describing the first prototype, Robert says he milled out a spherical container from modelling foam to create what is called an integrating sphere – a device used to generate total reflection and diffraction of light to analyse bacterial solutions placed inside it. The next version was 3D printed, about the size of a softball, and covered in tinfoil. "It looked a bit like the Death Star,” he says. They then moved to more of a jacket device, where “the integrating space basically hugs the vessel containing the bacteria and then we pass a laser beam through that and collect the data.” Essentially, as the laser light passes through the sample, it scatters. The light detected at the collector indicates the state of the bacterial cell population – growth phase, lag phase, or cell death.
“The secret to the machine is [that] it’s rapid because it’s sensitive. Generally speaking, it gets results for most organisms in under 30 minutes,” he says. This impressive speed comes thanks to its sensitivity. “It can see as few as 25 organisms in two millilitres of liquid – that’s the equivalent of finding 20 Smarties around the Wembley Stadium.”
With no further development, Robert says the laptop-sized devices could directly replace the machines currently used in hospitals, giving results in a matter of minutes, rather than several hours. However, he and his team have shown that with some tweaks, their device can even directly analyse urine samples, without the lengthy sample preparation process required by the currently used machines. “So that time from patient delivery of sample to result is significantly less than an hour, which is completely game-changing,” Robert says. “For blood, we need to slightly process the sample beforehand, but that takes no more than about five minutes.” Because microbes are usually found at a much lower concentration in the blood, the device takes a bit longer to produce a result – two to three hours, but this is still much less than the usual 48 hours.
So, what would this enable, going forwards? One big win is that doctors could ensure they give patients the correct antibiotic in the first instance, with evidence to back up any decisions made. This could help them avoid prescribing powerful antibiotics that have toxic side effects (in cases where they’re unsure if a less toxic one would work). For example, rifampicin, which is used to treat tuberculosis, can really damage the liver and turns the whites of the eyes red. Giving a less toxic drug to patients would prevent such side effects. “[The technology to enable this] exists, but it’s just not used. With my machines, if they’re rolled out, they’ll make the access to that data a lot simpler,” says Robert.
Old plus old equals new
Another fascinating application he and his team are working on is entirely new: analysing bacteria and drugs interacting. Bacterial growth patterns are well known. For example, if they’re multiplying rapidly, this is known as the log phase. Conversely, when bacteria are introduced to a new environment, they typically stop growing, entering what’s called a lag phase, while they adapt to the new environment. With the SLIC, Robert and his team have shown introducing a drug to resistant bacteria during a growth phase can interrupt it and cause a lag phase, making them more vulnerable to other drugs. “We will know if you administer drug X, then you know two hours later, you should administer drug Y,” he says. “And that would be more effective than it would have been if you administered the drug Y a day later, for example.”
Combining antibiotics in this way is “just not done. Generally, we treat organisms infecting individuals with monotherapy,” says Robert. This almost always means a single drug at a high dose. “We’re gathering data that shows using combinations of drugs at timed points during an infection can have a synergistic effect – doubling, tripling or quadrupling the effectiveness of a given antibiotic over time in a patient.” He gives the example of superbugs that can produce enzymes that break down antibiotics called carbapenems – usually considered ‘drugs of last resort’, and currently under threat. “We’ve shown that if you use a carbapenem in combination with something else at a given time during its growth cycle, you will still kill that organism,” says Robert. This is called ‘resuscitating’ the drug, and according to Robert, is good for patients, who receive a much lower dose of the antibiotic, and therefore less severe side effects. “And it’s important for the wider community because it means we’re not generating antibiotic resistance,” he says.
The future certainly looks less bleak with this in mind. And on top of this innovative approach, Robert, his team, and their collaborators are also using the device to investigate other potential antibiotic compounds – including compounds related to existing antibiotics, whose chemical structures have been tweaked, and even known drugs whose antimicrobial activity has not yet been studied. “That would be a massive step forward for the industry and for general healthcare, because that will give us access to whole new families of drugs we never thought of before.”
Contributors
Florence Downs
Editorial Manager
Keep up-to-date with Ingenia for free
SubscribeRelated content
Health & medical
A gamechanger in retinal scanning
2006 MacRobert Award winner Optos rapidly became a leading medical technology company and its scanners have taken millions of retinal images worldwide. There is even a display at the Science Museum featuring the Optos development. Alastair Atkinson, of the award-winning team, describes the personal tragedy that was the trigger for the creation of Optos.

Kidney dialysis
Small haemodialysis machines have been developed that will allow more people to treat themselves at home. The SC+ system that has been developed is lighter, smaller and easier to use than existing machines.

Engineering polymath wins major award
The 2015 Queen Elizabeth Prize for Engineering has been awarded to the ground-breaking chemical engineer Dr Robert Langer FREng for his revolutionary advances and leadership in engineering at the interface between chemistry and medicine.
Blast mitigation and injury treatment
The Royal British Legion Centre for Blast Injury Studies is a world-renowned research facility based at Imperial College London. Its director, Professor Anthony Bull FREng, explains how a multidisciplinary team is helping protect, treat and rehabilitate people who are exposed to explosive forces.
Other content from Ingenia
Quick read

- Environment & sustainability
- Opinion
A young engineer’s perspective on the good, the bad and the ugly of COP27

- Environment & sustainability
- Issue 95
How do we pay for net zero technologies?
Quick read

- Transport
- Mechanical
- How I got here
Electrifying trains and STEMAZING outreach

- Civil & structural
- Environment & sustainability
- Issue 95